Queer and trans* identities being in the public eye can be a double-edged sword. While there is more acceptance and representation of trans* people in the media, there is also an onslaught of government bills that threaten the fabric of their existence. As a trans journalist, I wanted to make sure folks like me had a chance to speak on our issues for ourselves.
According to the 2018 Outlook Study by the Rainbow Coalition of Waterloo, 96 per cent of trans* people have heard that being transgender is “not normal.” Only 56 per cent of trans* patients are comfortable sharing their gender identity with their primary healthcare provider.
Marcus Yang is a trans man who has actively pursued physical and social transition for over two years. Since he moved to KW 11 years ago with his family, Yang has since been entrenched in the local healthcare system.
“We had no reason to think there was a support group or an LGBT general mental health support group. There was some help center in downtown Kitchener but that has been closed for at least the past year. And I’ve not heard of a new one opening up,” Yang said.
So how can our region serve the underserved better? Taking a look at how trans healthcare is administered within the medical-industrial complex and ask how people learn about the healthcare options available to them. Being able to hear from those directly impacted can provide a look into what healthcare in the region as trans people to see what sort of experiences they have had, and what needs to be improved moving forward.
“I knew I was trans from a very young age, that kind of story. I was always more gender non-conforming and feminine for a long time. I didn’t think I was allowed to be trans because I was that way. It wasn’t until I was much older. And I started to glow. I got the courage to come out and be myself. That was about three years ago now,” trans community member Alister Stepowski said.
Having a gender dysphoria diagnosis is an important step for trans people to gain access to healthcare. Once a person has been officially diagnosed they are then able to seek other forms of medical transition. I was diagnosed with gender dysphoria in the fall of 2019. My own experience with being diagnosed was relatively easy compared to most, because I was lucky enough to have a doctor who was learned in helping trans* patients. Many folks know how hard it can be trying to find a new general practitioner. For trans individuals, this problem can be amplified.
“I think my partner at the time had mentioned it [the clinic]. Because they were non binary and had been looking for a clinic for themselves to use. And when I came out to them, they suggested it was a good idea. So it was just again, a really fortunate timing situation for me that I happened to be dating somebody who had already done all of the legwork for me,” Alex Cain said. Cain is a trans man who currently lives in the Waterloo Region. His current general practitioner is in St. Catherines which is where he was originally from. He has yet to find a healthcare provider he is comfortable with in the region.
There is no clear way to receive a gender dysphoria diagnosis in the Waterloo Region. When I decided to seek out going on hormone replacement therapy or HRT, I had started two years before I actually was ready. Based on what my other trans friends had said I knew it would take at least two years for me to start due to the medical red tape that exists. I am not alone in this experience.
“It definitely took some time. I think my family doctors generally asked some questions about I guess how I would describe my gender identity, whether or not like, and how much time I spent, like actually visibly presenting or for gender identifiers and how coming out and like what people’s reactions were and what my feelings were.” said Yang.
Trans people’s experiences can be as inconsistent as the healthcare system they exist in. Finding a physician who respects your gender can sometimes feel like a game of chance. There have been countless times I have gone into an appointment regarding my transition and being dead named at reception. According to the Rainbow Coalition, doctor’s offices are not considered one of the top five places where trans individuals feel safe.
“Oh, it’s really frustrating to know that any doctor in Ontario can prescribe hormones, but most of them just refuse to because it scares them. It’s such a non-invasive form of healthcare to know. It’s like a doctor not willing to prescribe birth control at this point. It’s weird. And to go through so many hoops to get to that is really frustrating,” Stepowski said.
Trans people are rarely afforded the spotlight and microphone when it comes to sharing our experiences. That is why as a trans journalist, I wanted to give people like me a voice, especially here in the KW region. There are some gender-affirming services such as SHORE and SPECTRUM that are available to the public. While the universities have Glow and The Rainbow Centre. However, the general consensus is that our healthcare for trans people has to be improved.
The Rainbow Coalition reported that 23 percent of trans people in the region have reported that their healthcare provider said they “do not know enough about trans-related care to provide it.” Public awareness also brings more misinformation and ignorance regarding hot button issues like trans rights.
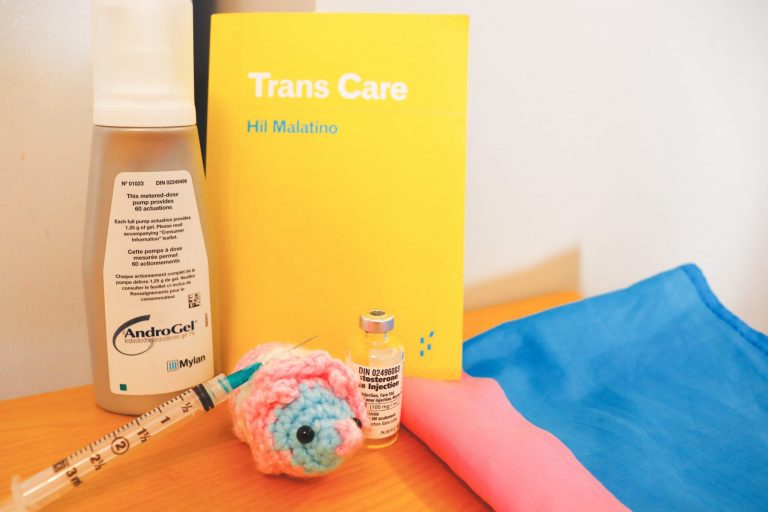
In his book, “Trans Care,” Mil Malantino called this phenomenon “surviving trans antagonism.”
“I think there needs to be a lot more education provided to health care providers about trans experiences. One of the reasons I’ve had so much anxiety about finding a doctor in the Kitchener Waterloo Region, is because anytime I’ve had to seek medical services as well here for completely valid transition-related issues. It has become all about my transition,” Cain said.